
The healthcare industry stands at a critical stage. Although artificial intelligence promises to revolutionise patient care, reduce costs, and address workforce shortages, a sobering reality emerges from boardrooms across the NHS and private healthcare organisations: 80% of AI projects fail to scale beyond the pilot phase.
For industry leaders who have witnessed promising demos turn into expensive disappointments, this failure rate is more than wasted resources – it signals a systemic challenge that threatens the sector’s ability to harness AI’s benefits.
The Real Problem: What Works in Labs Fails in Hospitals
The journey from AI demo to clinical deployment reveals a harsh truth.
Oleh Petrivskyy, CEO of Binariks – a global technology consulting and engineering partner with deep expertise in healthcare AI – has seen these challenges up close.
“Look, we have calls and meetings with healthcare organisations all the time telling us the same story – their AI pilot worked beautifully in controlled settings, but the moment they tried to use it with real patients and real doctors, everything fell apart,” explains Oleh Petrivskyy.
The core issues manifest in three critical areas:
- Data reality gap: Proof-of-concept projects rely on carefully curated datasets – clean and standardised. Production systems must contend with fragmented data across multiple EHR systems, inconsistent formats, and inevitable gaps in clinical workflows. A diagnostic AI achieving 95% accuracy on lab datasets might struggle to maintain 70% accuracy when processing real patient data.
- Infrastructure complexity: Legacy systems dominate healthcare IT landscapes, with many organisations running critical applications on decade-old hardware. These systems weren’t designed for modern AI workloads, creating performance bottlenecks that weren’t apparent during small-scale pilots.
- Workflow integration challenges: Clinical environments involve multiple stakeholders with competing priorities, including clinicians focused on patient care, IT departments managing system stability, and administrators controlling budgets.
The Three Barriers Killing Healthcare AI Projects
So why do so many promising pilots fail to scale in real-world clinical settings? We asked Oleh Petrivskyy to share firsthand insights into the biggest obstacles organisations face when moving from controlled lab results to everyday hospital operations.
These barriers are interconnected and are the most common:
- Technical barriers
- Integrating AI with fragmented, legacy systems and inconsistent data sources is tough; 30% of leading organisations cite it as the top challenge. What works in controlled settings often fails in live hospitals, with models prone to accuracy loss and performance drift when exposed to real-world complexity.
- Regulatory barriers
- Healthcare is highly regulated, with evolving privacy and compliance demands. Meeting data security and interoperability standards requires ongoing investment and a proactive compliance strategy from day one.
- Organisational barriers
- Even the best AI can’t succeed without clinical buy-in and long-term investment. Change management, cross-departmental coordination, and user training are critical – otherwise, AI tools risk becoming shelfware.
“The most technically perfect AI system will fail if the nurses hate using it or the doctors don’t trust it,” emphasises Oleh Petrivskyy.
“At the end of the day, it’s all about people. What we’ve learned is that getting buy-in from everyone who’ll actually use the system is way harder than most organisations expect, and they usually don’t plan for it.”
Breaking the Cycle: A Structured Approach to AI Scaling
Drawing from extensive experience working with healthcare clients who need rapid AI implementation while avoiding common pitfalls, Oleh Petrivskyy shares that Binariks has developed a specialized AI Centre of Excellence* division.
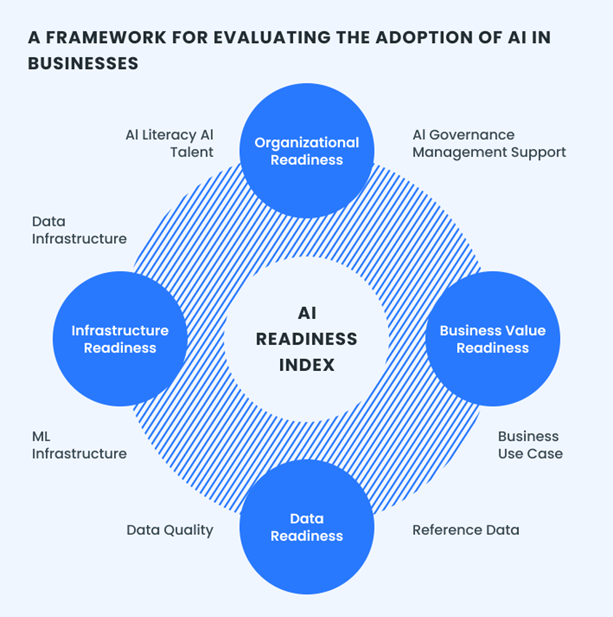
This framework addresses the unique challenges organisations at different levels of AI readiness face when adopting or scaling AI solutions beyond pilot projects.
“After working with dozens of healthcare organisations, we’ve seen the same pattern over and over – they try to implement AI the same way they’d roll out any other IT system, and it just doesn’t work,” explains Petrivskyy.
“That’s why we created our AI CoE – to give organisations the roadmap and support they need to actually succeed in production.”
A proven framework for AI success
- Evaluate & align
The team assesses the organisation’s current state across AI understanding, business needs, and data readiness. This includes comprehensive stakeholder mapping that extends beyond traditional IT participants to include clinical champions, compliance officers, and patient representatives.
- Explore & prototype
Rather than jumping into development, AI CoE experts identify high-value use cases and validate technical viability using the client’s data.
“Here’s what killed many AI projects: everyone’s excited about different things. The IT team wants cutting-edge tech, the doctors want something that makes their lives easier, and the executives want ROI. When these groups aren’t aligned, the project dies,” notes Oleh Petrivskyy.
“Our AI CoE basically gets everyone in the same room and makes sure they’re all working toward the same goal before anyone writes a single line of code.”
- Implement & integrate
The framework employs phased rollout strategies that allow iterative improvement whilst maintaining system performance. This approach includes:
- Automated data quality monitoring with privacy-preserving processing techniques
- Continuous performance tracking covering technical metrics and clinical outcomes
- Robust governance protocols addressing quality, security, and compliance from the outset
- Optimise & evolve
Production AI systems require ongoing monitoring and improvement. Binariks’ framework includes automated systems tracking model performance, data quality, user adoption, and clinical outcomes.
Cost-effective implementation
“The biggest myth in healthcare AI is that you need millions of dollars to start. That’s just not true. But you need to be smart about where you spend your money,” notes Petrivskyy.
In particular, organisations can maximise value through:
- Cloud-based solutions, where appropriate, avoiding unnecessary infrastructure costs
- Strategic partnerships: Development firms’ strategic cloud partnerships can provide organisations with significant savings through programmes like AWS Activate
- Reusable components: Building standardised processes applicable across multiple AI projects
- Optimal tool selection: Choosing between custom development and proven cloud solutions only based on specific estimations
“As for Binariks, we’re not in the business of building custom solutions just because we can. If there’s a tool that already does what you need and costs a fraction of the price, we’ll tell you to use that instead,” explains Oleh Petrivskyy.
“The clients who see the best results? They’re not trying to revolutionize healthcare overnight. They pick one specific problem, solve it really well with AI, and then move on to the next one.”
Timeline and resource expectations
Scaling AI in healthcare isn’t a quick win but a long-term journey, which makes realistic expectations crucial for success. The timeline varies dramatically based on project complexity and regulatory requirements. For example:
- For operational optimization projects, such as scheduling automation or clinical note processing, expect 3-4 months for implementation.
“When planning AI projects, we recommend focusing on 3-4 month horizons for non-regulated solutions,” says Oleh Petrivskyy. “The reality is that AI evolves so rapidly that longer development cycles risk being overtaken by ready-made solutions.”
- Clinical decision support systems requiring regulatory compliance demand 9+ months minimum, primarily for certification preparation and extensive documentation.
- Complex domains like biotech face additional challenges, as solutions in these areas cannot be delivered quickly. Testing must be conducted by subject matter regulatory experts (SMEs), and the development speed itself becomes irrelevant. What matters is when SMEs confirm the system performs adequately and how many iterations are required to reach an acceptable level of functionality.
The key consideration: if your system handles sensitive data or requires compliance approvals, budget significantly more time. For non-regulated operational improvements, maintain agility with shorter development cycles to stay aligned with the fast-paced AI landscape.
P.S. From Pilot Purgatory to Production Success
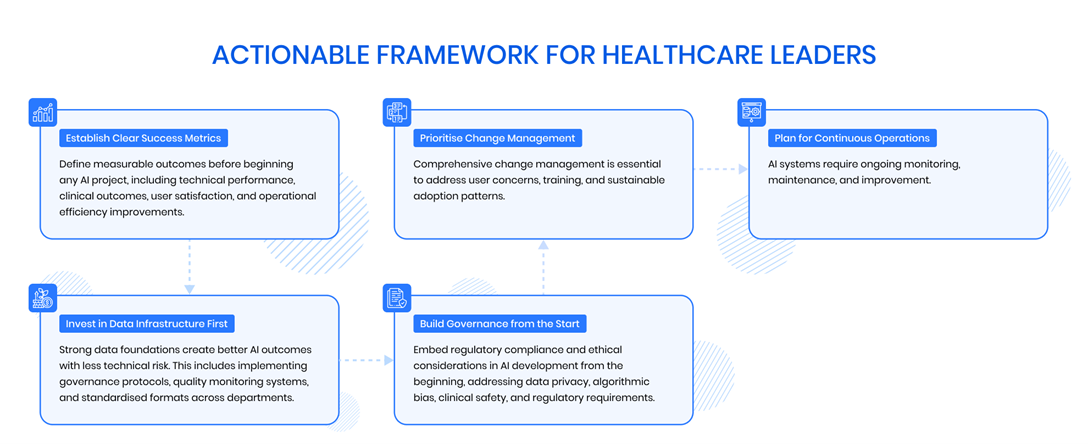
The 80% failure rate for healthcare AI projects isn’t inevitable. Organisations successfully bridging the implementation gap achieve substantial competitive advantages and clinical improvements.
“If you want to escape the pilot trap, you can’t just throw better technology at the problem. You need to completely change how you think about implementing AI,” concludes Oleh Petrivskyy.
“Start with scaling in mind, deal with the people and policy issues right alongside the technical stuff, and keep your expectations realistic. Do that, and you won’t just add AI to your toolkit – you can truly change how your organisation operates.”
Today, the choice for healthcare leaders is clear: continue the cycle of promising pilots that never reach production, or adopt the comprehensive approach needed to bridge the implementation gap.
The technology exists. The business case is proven. The framework for success is available.
The question is: will your organisation be among the 20% that succeed?
*Binariks’ AI Centre of Excellence helps healthcare organisations scale AI implementations across the US, UK, and Europe. For more information on bridging the healthcare AI implementation gap, visit binariks.com or contact their healthcare AI specialists.











