The old saying goes: “Prevention is better than cure.” Yet according to one scientific study, our relatively primitive human brain has not yet properly evolved to enable us to naturally plan and make provisions for life in the distant future.
This means we are prone to taking daily risks. We give little regard to the impact our behaviour and habits will have on our quality of life as we enter old age, and so we continue to eat excessively, drink excessively and do all the other indulgent things we’re told not to do because the likely consequences are but a tiny dot in the distance of our mortal lives.
There are, of course, always exceptions to the rule; there are people who fear surprises and carefully plan and put safeguards in place for every kind of eventuality. But the majority of us will still shy away from visualising our future older self; even as the danger of dependence, loneliness and impoverishment in old age becomes a greater possibility even to those currently living a comfortable, healthy, middle-class life.
But what if technology can predict, prevent and manage illness – especially age-related ones – long before they escalate into conditions that require hospitalisation, and long before we ourselves become a burden to the care system and to our families? Developments in health technology have slowly been emerging to innovate and solve a prominent human problem that has, for too long, been ignored to the point that it’s become the ‘new climate change’.
It is precisely this vision of ‘prevention is better than cure’ optimised by a tech-enabled public health service that Health Secretary Matt Hancock has been heavily positing, in recent speeches, as a solution to protecting the sustainability of the NHS. Though his proposals to empower people to take responsibility for their own health is not without critics, the vision signifies an intention and willingness to alleviate pressure off a crumbling system relied upon by some of society’s most vulnerable.
Last year, the UK endured a particularly bitter winter that led to an unprecedented number of hospital admissions, bed shortages, patient waiting times and delays in hospital discharges – largely affecting those aged 65 and over. According to recent NHS figures, almost 1,000 elderly people a day were hospitalised for simple conditions that, if identified and managed effectively, would not require hospitalisation. More disturbingly were the National Audit Office’s analyses of the effects of such unnecessary hospital admissions. It concluded that, with a 10 day stay in hospital, a patient’s health would have deteriorated to such a point that their life expectancy was reduced by as much as ten years. It is clear that the future of ‘health’ – especially for older people – lies at home, not at hospital – at least in the general sense.
My journey into ‘agetech’ is a personal one. Years back, when I was just a teenager, I had witnessed my own grandfather put into a residential care home at the stage where his Parkinson’s disease became too difficult for him to manage living independently. But he hated being there and it was hard seeing him this way – the once happy, strong and playful grandfather I once knew in childhood reduced to nothing more than a shadow of his former self. Would he have been more ‘himself’ had the provisions been available to allow him to continue living safely in the comforts of the house he once shared with his family? I have no doubt.
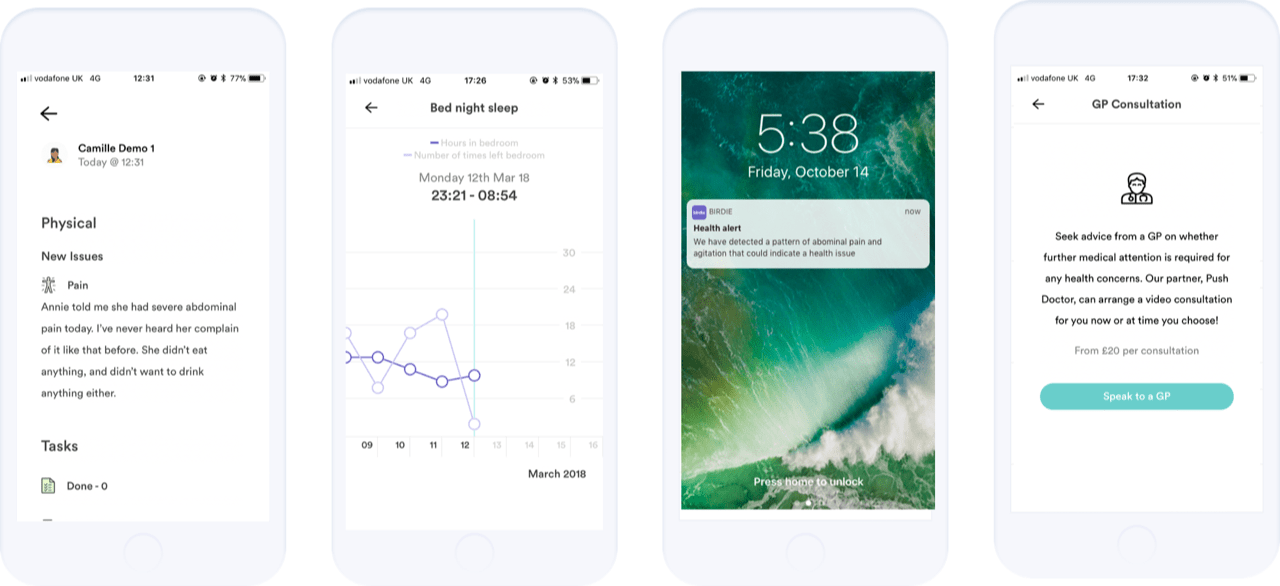
A ‘connected home’ would’ve ensured that he could navigate his environment independently, safe in the knowledge that – should he have a fall – assistance would be deployed instantly. Door sensors around the house would’ve tracked his movements and behaviour and flag anything seemingly untoward or unusual that could signal physical or emotional distress. For example, detected acute confusion combined with increased bathroom visits logged by such sensors could potentially indicate a urinary tract infection – one of the major causes for admissions into hospital in the elderly – but a condition that is simple to manage if identified at an earlier stage. Decreased physical activity in the home, more so than usual, could indicate weakness or impairment of some kind. An app would’ve enabled his carer to check in, document and share information from the daily routine check-ups directly with the care organisation and the various clinicians managing his care, and his closest family would be privy to that information too; they would be instantly notified via the app whether a carer had come and gone and if there was any cause for concern.
It is this kind of capability – machine learning through connected and mobile devices with critical human input – that has formed the basis for the very kind of technology we’re pioneering. Predictive analytics empower the correct people in the circle of care with instantly actionable real-time data. Access to this kind of knowledge allows issues to be dealt with before they become serious or life-threatening problems.
When we initially started researching tech-enabled solutions to the ageing problem, alongside speaking to hundreds of patients, families, care professionals, care providers, doctors and geriatricians, there was one particular insight that struck me. The geriatricians believed that emergency admissions into hospitals in elderly people could be lowered by as much as 20 per cent if there was better communication between clinicians and care professionals based on hard data of the kind that is garnered by connected devices and the frontline care staff. Imagine what this could mean in terms of improving quality and longevity of life in society’s most vulnerable; in driving standards of domiciliary care up; in easing pressure off the NHS; and in giving families peace of mind.
We can’t stop the clock turning. We can’t stall or prevent ageing. But, in the age of AI and driverless cars, we can improve the experience and change the concluding chapters of a typical older person’s life. It is our natural human defence to shy away from visualising the terrifying eventualities of old age. But empowering technology has the ability to help us override this fear, change our approach to dealing with ageing and build a better society that enables us to age with confidence, on our own terms.
Max Parmentier is CEO and founder of Birdie – a holistic home care platform that empowers older adults to live at home independently for longer. The venture is backed by AXA and recently raised €7m Series A to scale its product nationwide and innovate the home care sector.